What is sleep-disordered breathing (SDB)?
SDB describes a number of nocturnal breathing disorders:
- Obstructive sleep apnea (OSA)
- Central sleep apnea (CSA)
- Nocturnal hypoventilation
- Cheyne–Stokes respiration (CSR)
What is obstructive sleep apnea (OSA)?
- The most common form of SDB
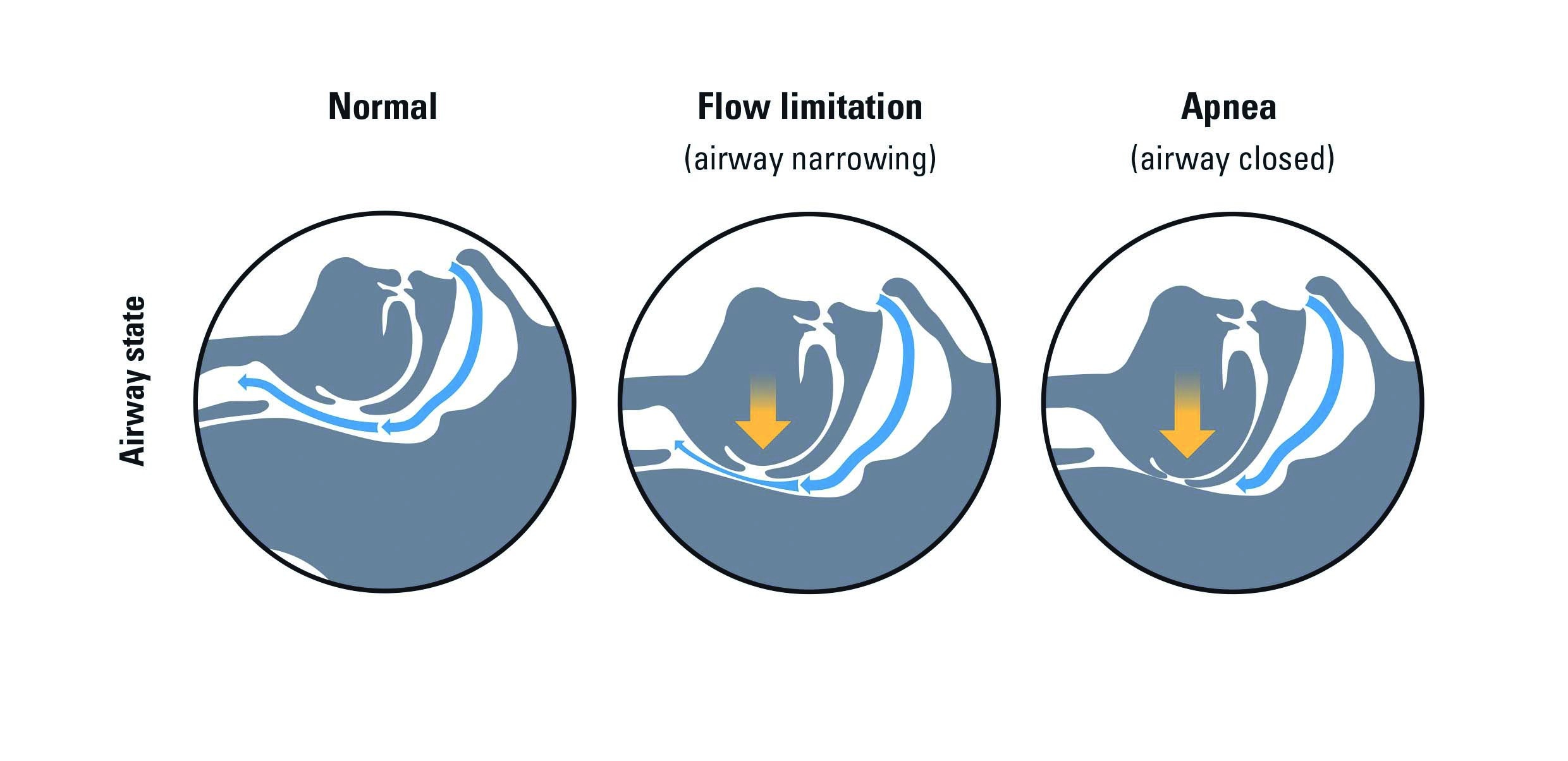
- A partial or complete collapse of the upper airway caused by relaxation of the muscles controlling the soft palate and tongue
- Person experiences apneas, hypopneas and flow limitation
- Apnea: a cessation of airflow for more than ten seconds
- Hypopnea: a decrease in airflow lasting more than ten seconds with a 30 percent reduction in airflow and at least a three percent oxygen desaturation from the baseline
- Flow limitation: narrowing of the upper airway and an indication of an impending upper airway closure
Signs and symptoms of sleep apnea?
- Lack of energy
- Morning headaches
- Frequent nocturnal urination
- Depression
- Excessive daytime sleepiness (EDS)
- Nighttime gasping, choking or coughing
- Gastroesophageal reflux (GE reflux)
- Irregular breathing during sleep (e.g., snoring)
Classification of sleep apnea
Apnea–hypopnea index (AHI)
- Number of apneas and/or hypopneas per hour of sleep (or study time)
- Reflects the severity of sleep apnea
AHI: less than five Normal range
AHI: five to less than 15 Mild sleep apnea
AHI: 15 to less than 30 Moderate sleep apnea
AHI: 30 Severe sleep apnea
Prevalence of sleep apnea
- Approximately 42 million American adults have SDB1
- An estimated 26 percent of adults have at least mild SDB2
- Nine percent of middle-aged women and 25 percent of middle-aged men suffer from OSA3
- Prevalence in the US is similar to asthma (20 million) and diabetes (23.6 million)4
- 75 percent of severe SDB cases remain undiagnosed5
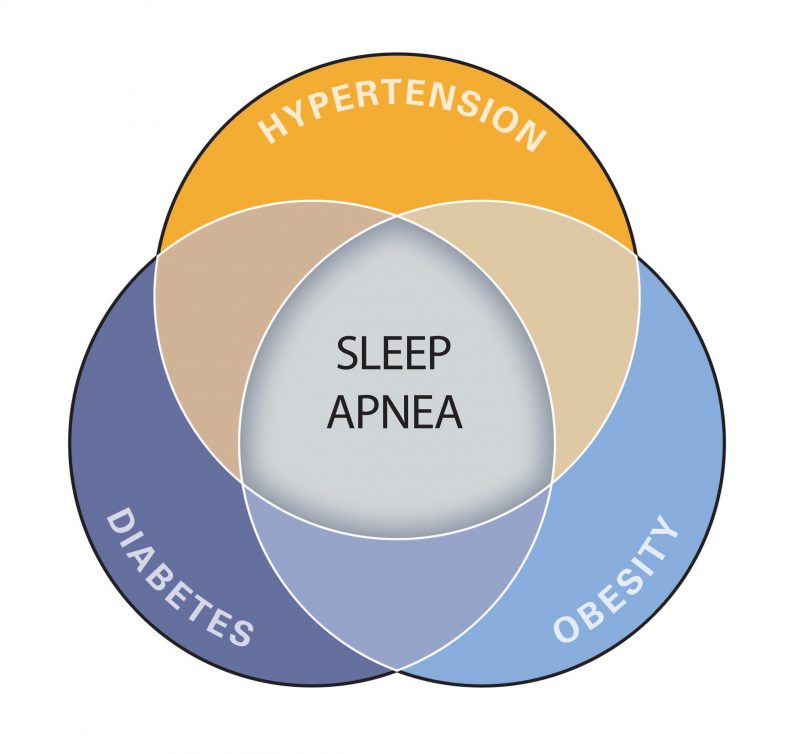
Increased risk factors for sleep apnea
- Obesity (BMI >30)
- Diagnosis of hypertension
- Large neck circumference (>17” men; >16” women)
- Male gender
- Excessive use of alcohol or sedatives
- Upper airway or facial abnormalities
- Smoking
- Family history of OSA
- Endocrine and metabolic disorders
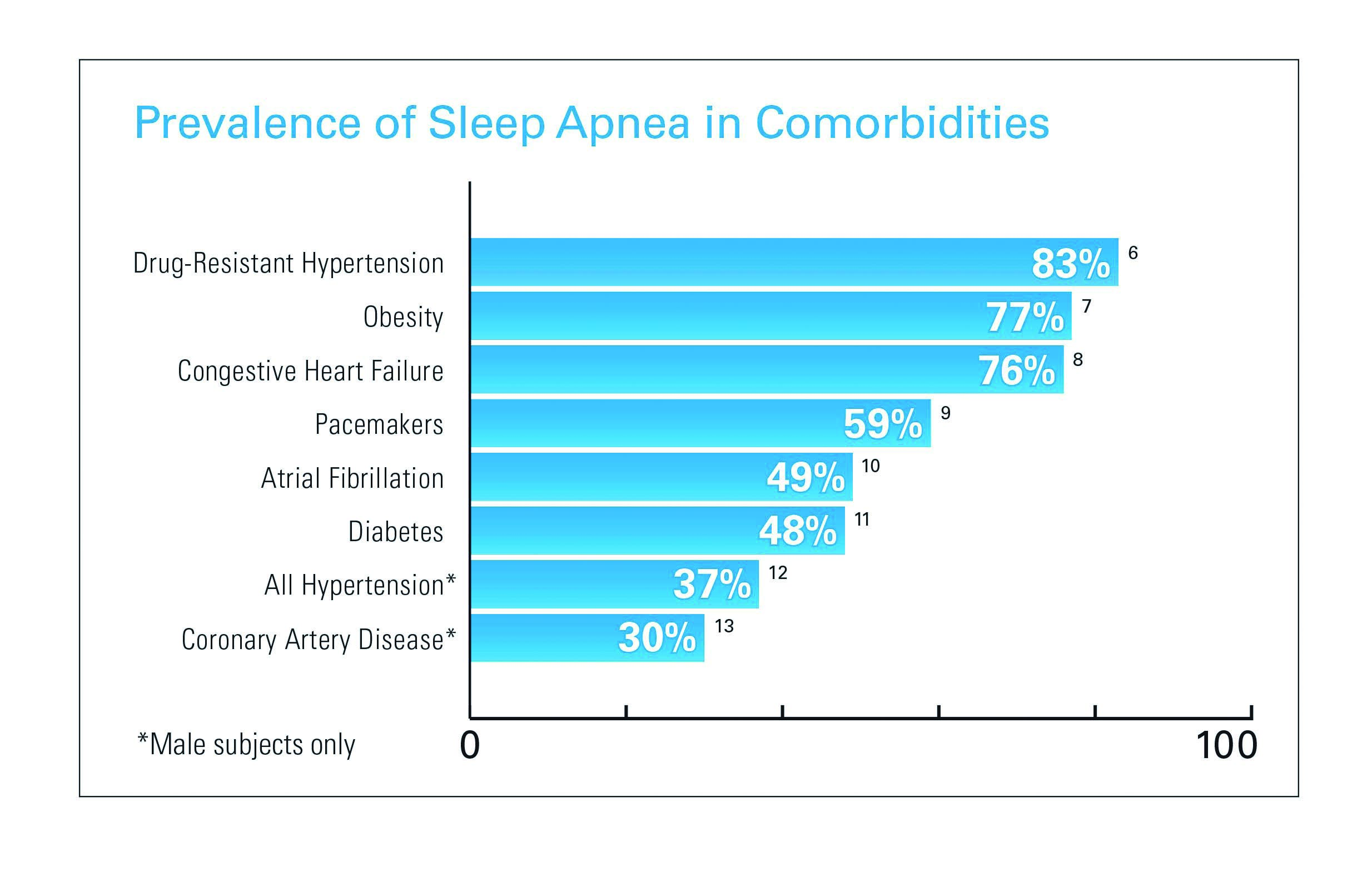
Cardiovascular links
- 1 million people in the US have heart failure14
- Approximately 76 percent of congestive heart failure patients have SDB8
- Heart failure is the most expensive disorder to treat15
- OSA noted in 49 percent of atrial fibrillation patients10 and 30 percent of cardiovascular patients13
- OSA presents in 70 percent of heart attack patients with AHI greater than five and 52 percent of heart attack patients with AHI greater than ten16
Hypertension links
- Studies have shown that sleep apnea is an independent risk factor for hypertension
- 30–83 percent of patients with hypertension have sleep apnea6,12
- 43 percent of patients with mild OSA and 69 percent of patients with severe OSA have hypertension5
- AHA guidelines on drug-resistant hypertension have shown that treatment of sleep apnea with CPAP is likely to improve blood pressure control
Type 2 diabetes links
- 48 percent of type two diabetes sufferers have sleep apnea11
- OSA may have a causal role in the development of type two diabetes17
- OSA is associated with insulin resistance (independent of obesity)18
- 30 percent of patients presented to a sleep clinic have impaired glucose intolerance19
- Mild forms of SDB may be important in predicting risk of pre-diabetes20
- 86 percent of obese type two diabetic patients suffer from sleep apnea21
Stroke risk
- 65 percent of stroke patients have SDB22
- Moderate to severe sleep apnea triples stroke risk in men23
Mortality links
- SDB is associated with a threefold increase in mortality risk5
- There is an independent association of moderate to severe OSA with increased mortality risk3
- Severe sleep apnea raises death risk by 46 percent24
Health care costs (Economic consequences of untreated SDB)
- Patients with untreated OSA had 82 percent higher in-patient hospital costs than treated patients25
- Patients with OSA have higher utilisation rates and incur greater costs than non-OSA patients for up to ten years prior to diagnosis26
- OSA patients on PAP therapy have 31 percent lower total medical costs than patients not on PAP therapy25
Traffic accidents
- In the year 2000, 810,000 US drivers were involved in a motor vehicle accident related to OSA – 1,400 involved fatalities27
- Treating all US drivers suffering from sleep apnea would save US$11.1 billion in collision costs and saves 980 lives annually27
Treatment of OSA with CPAP
- CPAP treatment reduces the need for acute hospital admission due to cardiovascular disease in patients with sleep apnea28
- CPAP reduces blood glucose levels29
- Two nights of CPAP improves insulin sensitivity, sustained at the three-month interval30
- For every dollar spent on CPAP, US$3.49 would be saved in reduced collision costs27
For more information get in touch with:
- PT ResIndo Medika
- Graha BIP, 5th Floor
- Jl. Jend. Gatot Subroto Kav. 23
- Jakarta 12930
- Indonesia
- Phone: +62-21 525 8230-31
- Fax : +62-21 252 1380
- Mobile: +62-856 802 8888
- +62-812 8853 1052
References:
- Young et al. New Engl J Med 1993
- Peppard et al. J Am Med Assoc 2013
- Marshall et al. Sleep 2008
- US Department of Health and Human Services, Centers for Disease Control and Prevention 2008
- Young et al. Sleep 2008
- Logan et al. J Hypertens 2001
- O’Keeffe & Patterson. Obes Surg 2004
- Oldenburg et al. Eur J Heart Fail 2007
- Garrigue et al. Circulation 2007
- Gami et al. Circulation 2004
- Einhorn et al. Endocr Pract 2007
- Sjostrom et al. Thorax 2002
- Schafer et al. Cardiology 1999
- Go AS, et al. American Heart Association 2013
- Medicare – $20.4 billion p.a.
- Kuniyoshi et al. J Am Coll Cardiol 2008
- 17 Reichmuth et al. Am J Respir Crit Care Med 2005
- 18 Punjabi et al. Am J Respir Crit Care Med 2002
- Meslier et al. Eur Respir J 2003
- Stamatakis et al. Sleep 2008
- Foster et al. Diabetes Care 2009
- Dyken et al. Stroke 1996
- Redline et al. Am J Respir Crit Care Med 2010
- Punjabi et al. PLoS Medicine 2009
- Potts et al. Popul Health Manag 2012
- Albarrak et al. Sleep 2005
- Sassani et al. Sleep 2004
- Peker et al. Am J Respir Crit Care Med 1997
- Babu et al. Arch Intern Med 2005
- Harsch et al. Am J Respir Crit Care Med 2004